2020B15 Discuss factors that determine the time to awakening after cessation of a propofol target infusion (TCI).
List:
· Emergence modelling
· Uptake
· Elimination
· Threshold
Emergence modelling:
|
Determinants |
1. Uptake (into all compartments) 2. Elimination (from effect site via central compartment) 3. Threshold (median effect site concentration for emergence – i.e. Ce50) |
||||||||||||
|
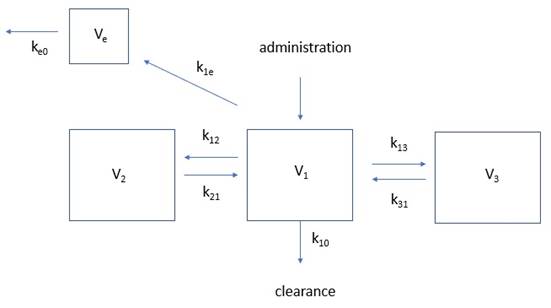
Kinetic model |
|
||||||||||||
|
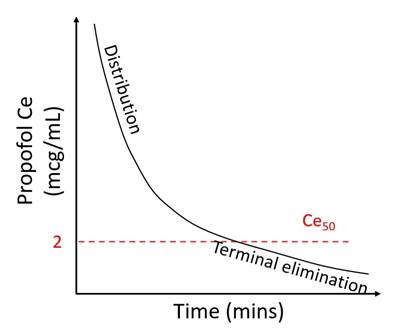
Washout curve |
Half lives: · t1/2α fast: 2 mins · t1/2α slow: 20-50 mins · t1/2β: 5-12 hours
|
||||||||||||
|
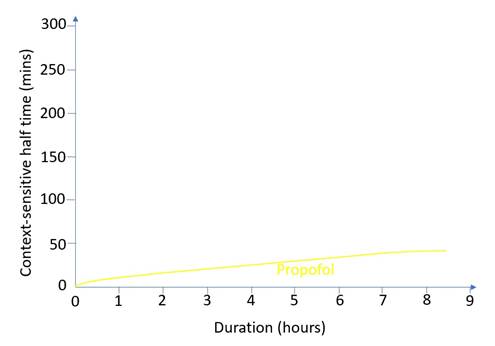
Decrement times |
· Fast offset after short infusion · Slow offset after long infusion
|
1. Uptake (factors increasing it)
|
Infusion |
· ↑Duration · ↑Infusion rate / target concentration |
|
Patient |
· ↑Cardiac output -> ↑tissue blood flow (child, pregnant, obese, septic) · ↑Compartment volumes -> ↑capacity (lean tissue, fat) |
|
Algorithm |
· Marsh > Schnider · Male > female · ∝ weight, height, youth |
|
Logistics |
· Factors impeding titration: o Neuromuscular blockade o Absence of processed EEG |
2. Elimination (factors slowing it)
|
Short case |
Offset during distribution phase: · ↓Distribution to V2, V3 o ↓Cardiac output (old age, heart failure, hypovolaemia) o ↓Compartment volumes (cachexia) |
|
Long case |
Offset during terminal elimination phase: (note bivalent factors!) · ↑Redistribution from V2, V3 o ↑Cardiac output o ↑Compartment volumes · ↓Metabolism (↓mAP -> ↓hepatic blood flow; liver disease if severe) · ↓Excretion (<1%) |
3. Threshold (factors lowering it)
|
Pharmacology |
· Synergistic: opioids, benzo · Additive: sevoflurane, N2O |
|
Physiology |
· Old age · Pregnancy (↓30%) · Night time (↓10%) |
|
Pathology |
· ↓↓PaO2 · ↑↑PaCO2 · ↓↓mAP · ↓↓pH · ↓↓Temp |
Feedback welcome at ketaminenightmares@gmail.com