2013A11 Compare and contrast lung function in the neonate with that of an adult
List:
· Definitions
· Anatomy
· Lung volumes
· Resistance and compliance
· Ventilation and perfusion
· Gas exchange
· Control of ventilation
· Other
Definitions:
Neonate: <4/52 old, born 37-40/40
Adult: >18 years
Anatomy:
|
Anatomical feature |
Clinical implication |
|
Upper airways: |
|
|
Narrow upper airways: · Narrow nasal passages · Large tongue · Narrow pharynx |
↑ Resistance · Provides auto-PEEP · Any obstruction = dangerous |
|
Obligate nose breather because of · Big tongue · High laryngeal inlet (C3-4 cf. C6) |
· Any obstruction = dangerous |
|
Prominent occiput |
· Tendency for flexion -> obstruction · No need for pillow for bag & mask, intubation |
|
|
|
|
Lower airways: |
|
|
Narrower lower airways · Narrower larynx, trachea and bronchi · Note narrowest point cricoid ring (cf. glottis in adults) |
· Obstruction = dangerous · Use uncuffed ETT |
|
· Epiglottis long, U shape, floppy |
· Use straight blade |
|
· Laryngeal inlet is high C3-4 and anterior |
· Different intubation mechanics |
|
· Short trachea |
· Endobronchial intubation common |
|
|
|
|
Chest wall |
|
|
· Horizontal, cartilaginous ribs · ↓Outward recoil · ↓Bucket handle motion · ↓AP and lateral expansion |
· Almost all diaphragmatic breathing · Abdo constriction dangerous · ↑Airway collapse in expiration · FRC < closing capacity |
|
Resp muscle: ↓type 1 fibres · Diaphragm: 20% diaphragm cf. 55% adult · Intercostals: 45% diaphragm cf. 65% adult |
· ↓ reserve · ↑ risk type 2 respiratory failure |
Lung volumes:
|
Volume |
Implication |
|
· VT 7mL/kg in both |
|
|
· VD 2.2mL/kg in both |
|
|
· FRC 30mL/kg supine in both. |
|
|
· *Note FRC < closing capacity in neonates |
· Gas trapping |
|
· *Note FRC ↓↓ under GA · (muscle relaxation -> outward recoil) |
· Rapid desaturation (also because ↑metabolic rate) |
|
· FVC cannot accurately be measured in the neonate |
|
|
· TLC 50mL/kg neonate cf. 70mL/kg adult |
|
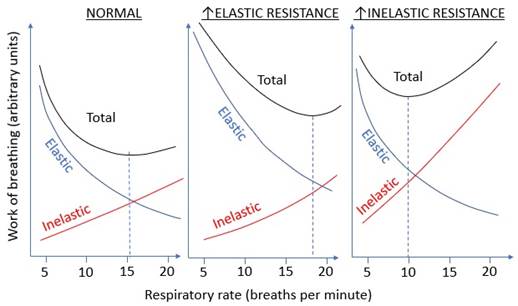
Resistance and compliance
|
Parameter |
Implications: |
|
Static compliance: · 1.5-6mL/cmH2O neonate · 100mL/cmH2O adult Specific lung compliance: no change Chest wall compliance: · Higher than in adults |
Neonate ↑RR for ↓work of breathing · Resistance 15x higher · Compliance 20x lower
|
|
Dynamic compliance: adult > neonate · ↑AWR neonate |
|
|
Specific compliance = static compliance/FRC: · Same in neonate and adult |
|
|
Airway resistance: · 25cmH2O/L/s on day 2, cf. adult 2cmH2O/L/s |
Ventilation and perfusion:
|
Parameter |
Implication |
|
· RR 12 in adult, 40 in neonate · VT 5-8mL/kg both |
· ↓Reserve for ↑RR |
|
· MV 220mL/kg/min neonate, 110mL/kg/min adults · VA 140mL/kg/min in neonate, 70mL/kg/min adult · Due to 2x ↑VO2 (7-8mL/kg/min) |
· ↑Work of breathing |
|
· ↑Cardiac output 140mL/kg/min |
· ↑pulmonary blood flow |
Gas exchange:
|
Difference: |
Implication |
|
(1)↑ O2 consumption: 7-8mL/kg/min in neonates, 3-4mL/kg/min in in adults |
· Rapid desaturation in apnoeic neonates |
|
(2)↓ PaO2: 50-70mmHg neonate, 100mmHg adult Due to: · VQ mismatch: 0.4 neonate (due to FRC <CC), 0.8 adult · R->L shunt: 10% neonate, 2-3% adult (??) |
· ↓CaO2 · ↓Reserve in illness e.g. pneumonia |
|
(3)↑O2 carrying capacity · [Hb] 17-18g/dL cf. 12-14g/dL · HbF p50 19mmHg cf. HbA p50 27mmHg |
· Partly offsets ↓PaO2 such that CaO2 16mL/100mL c.f. 20mL/100mL · Increases blood viscosity hence afterload |
Control of ventilation:
|
Difference |
Implication |
|
· Immature respiratory centre in neonates · Depressed by hypothermia |
· Frequent mild apneas · ↑Frequent ↑duration post-op |
|
Acid-base neonate: · CO2-MV response curve left shifted · Compensated resp alkalosis |
· ↓Reserve for ↑ventilation |
Other:
|
Neonate specific oxygen toxicity |
· Retinopathy of prematurity · Bronchopulmonary dysplasia · Necrotising enterocolitis |
|
Non-respiratory functions |
· Innate immunity e.g. mucocilicary escalator present in neonate and adult · Adaptive immunity: passive (from breast milk) vs endogenous. No endogenous IgG or IgA in neonatal alveolar lining fluid |
|
Response to stress |
· ↓PaO2, ↑PaCO2, ↓pH -> ↑PVR -> reversion to foetal circulation -> hypoxia |
Feedback welcome at ketaminenightmares@gmail.com